Abstract:
This case study follows the journey of Ms. Johnson*, a 76-year-old female with bilateral profound sensorineural hearing loss, who utilizes a hearing aid, and is given recommendations for a cochlear implant by a clinical audiologist. She was initially seen at a hearing clinic with severe to profound sensorineural hearing loss and benefited from a monaural hearing aid for the left ear. However, her condition deteriorated over time, leading to significant communication challenges. After thorough assessment and consultation, it was recommended that Ms. Johnson consider seeking medical and clinical evaluation for a cochlear implant, which could ultimately allow her to experience substantial improvements in her hearing and quality of life.
This case study article will explore the clinical perspective on the challenges faced when hearing aids may not adequately address the needs of individuals with severe to profound hearing loss, outlining the clinical evaluation and process of transitioning from hearing aids to recommending a cochlear implant. Specifically, this article evaluates Ms. Johnson’s cochlear implant recommendations from the viewpoint of a professional clinical audiologist.
Introduction:
Hearing loss is a common sensory impairment that varies in severity, from mild to profound, and can result from factors like aging, genetics, and exposure to loud noise. Its effects extend beyond difficulty hearing to include challenges in communication, social interactions, and overall quality of life.
Incidence and Prevalence of Hearing Loss:
Hearing loss poses a significant health concern, particularly among older adults, impacting their ability to communicate effectively and enjoy life fully. With age, the likelihood of experiencing hearing impairment rises substantially (Shukla et al., 2020).
Around the globe, an estimated 466 million people, which is more than 6.1% of the world's population, have disabling hearing loss. In the United States alone, over 40 million individuals experience this condition, accounting for 4.6% of the population. For those aged 12 and above, about two million people have severe-to-profound hearing loss in both ears, making hearing loss the third most common chronic health issue in the United States (Zeitler et al., 2024).
Estimates suggest that around one in three individuals aged 65 and older encounter some degree of hearing loss. This prevalence increases with advancing age, with nearly half of individuals over 75 struggling with significant hearing difficulties (Zeitler et al., 2024).
Ms. Johnson’s Case History:
Mrs. Johnson has a history of gradually declining hearing over the past few months. She was initially seen at the clinic in 1992 with a known history of profound unaidable sensorineural hearing loss in the right ear and severe to profound sensorineural hearing loss in the left ear. Her hearing loss was of unknown etiology. She expressed at that time that she obtained decent benefits using her Oticon E39PL analog Behind-the-Ear (BTE) hearing aid. She stated then that her hearing aid assisted her in speech reading and with environmental awareness. However, she expressed difficulty hearing speech in all situations except in one-on-one conversations and in a quiet setting. She expressed that she would like to improve her communication skills with the help of her left hearing aid. She could not benefit from the use of amplification from her right ear due to the profound nature of her hearing loss. Ms. Johnson previously wore her Oticon E28PL analog hearing aid; however, it was broken beyond repair.
Although Ms. Johnson has managed her hearing loss with some success with a conventional superpower analog BTE hearing aid, she eventually transitioned to a programmable superpower BTE hearing. She then ultimately ended up with an ultrapower digital BTE hearing aid for her left ear.
Since 1992, she has been seen regularly for an updated hearing evaluation and hearing aid check, and obtaining a few new hearing aids for her left ear over some time. She was last seen in the Fall of 2023 for a hearing aid adjustment of her new ultrapower digital BTE hearing aid for her left ear. She expressed at that time that she was experiencing difficulty with the loudness (intensity) of sounds and understanding words. The hearing aid was adjusted to the maximum capabilities to provide Ms. Johnson with better comfort with speech understanding.
Ms. Johnson arrived at the clinic six months later for a hearing evaluation as recommended. She arrived with complaints that her hearing aid was no longer working for her left ear. Ms. Johnson stated that in recent months, she noticed a significant deterioration in her hearing abilities in her left ear, particularly when struggling in quiet and noisy environments and experiencing communication difficulties. Despite adjustments to her reasonably new hearing aid, she found minimal to no benefit, leading to frustration and social withdrawal.
Ms. Johnson’s Hearing Evaluation and Hearing Aid History (Timeline):
1992:
Ms. Johnson was first seen at the clinic in 1992 for a hearing evaluation. She presented with a known severe to profound sensorineural hearing loss in the right ear and severe to profound sensorineural hearing loss in the left ear. She reported that her hearing loss was due to unknown causes.
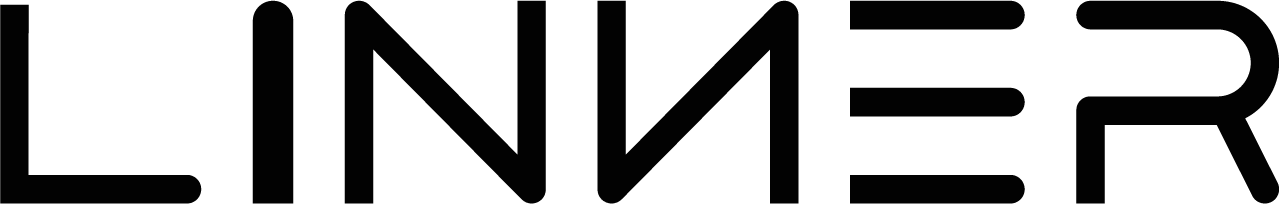
Ms. Johnson’s test results revealed profound sensorineural hearing loss bilaterally when measured from 250 Hertz (Hz) to 1500 Hz for the left ear and no responses to the level of the equipment for the right ear.
Ms. Johnson’s speech awareness threshold (SAT) was obtained at 75 decibel hearing level (dB HL) for the left ear and no measurable response in the right ear. Her word recognition score was obtained at 20% (poor word recognition ability) at the volume level of 105 dB HL. Her right ear word recognition could not be tested due to the profound nature of her hearing loss.

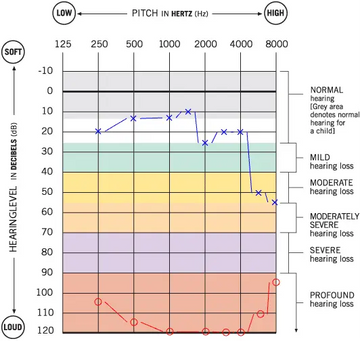
Ms. Johnson’s 1992 Audiogram
(Blue X’s= Left Ear, Red O’s=Right Ear)
Ms. Johnson was fitted with an Oticon E39PL analog BTE hearing aid for the left ear. The hearing aid has an on, off, and T-coil switch and a volume control wheel, which she kept between volume levels 2 and 3 for better listening comfort.

Oticon 39PL Analog BTE
1994:
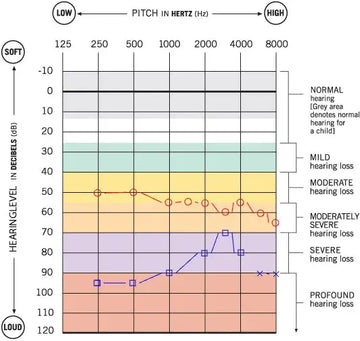
Ms. Johnson returned for her updated hearing test. At that time, testing revealed severe to profound hearing loss with responses from 125 to 1500 Hz for the left ear and no measurable responses for the right ear. Using her Oticon E39PL hearing aid, Aided testing in the soundfield revealed that Ms. Johnson functioned as an individual with mild to moderate hearing loss from 250 Hz to 1500 Hz and no measurable responses beyond 1500 Hz or in the higher frequencies due to the profound nature of her high-frequency hearing loss.
Ms. Johnson’s speech awareness threshold was obtained at 80 dB HL for the left ear, and no measurable response in the right ear. Her word recognition score was obtained at 24% (poor word recognition ability) at the volume level of 105 dB HL. Her right ear word recognition could not be tested due to the profound nature of her hearing loss.

Ms. Johnson’s 1994 Audiogram
(Blue X’s= Left Ear, Red O’s=Right Ear)
1995:
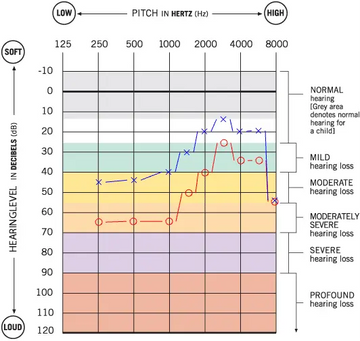
In 1995, Ms. Johnson’s test result revealed no significant changes in her hearing sensitivity (severe to profound hearing loss in the left and profound hearing loss in the right). Her hearing aid was tested in the booth, and it was revealed that Ms. Johnson continues to function as an individual with mild to moderately severe hearing loss from 250 to 1500 Hz with the use of her hearing aid. Ms. Johnson’s SAT remained stable compared to her 1994 test results (80 dB HL for the left ear and no responses for the right ear).

Ms. Johnson’s 1995 Audiogram
(Blue X’s= Left Ear, Red O’s=Right Ear)
2000:
Ms. Johnson returned to the clinic in 2000 for a new hearing test and to check her left hearing aid. She reported a noticeable decrease in her left hearing sensitivity since 1995. Her updated hearing test revealed profound sensorineural hearing loss bilaterally with a noticeably decreased hearing sensitivity in the left ear compared to her last test results. Her SAT was obtained at 95 dB HL with 40% word recognition ability at her most comfortable volume level of 100 dB HL.

Ms. Johnson’s 2000 Audiogram
(Blue X’s= Left Ear, Red O’s=Right Ear)
Ms. Johnson obtained AVR ImpaCt DSR 675 Programmable Analog BTE hearing aid. Like the Oticon E39PL hearing device, this hearing aid has an on and off switch and a volume control wheel. Ms. Johnson reported comfort with her hearing aid at the volume level of 3. 
AVR ImpaCt DSR 675 Programmable Analog BTE
2014:
Ms. Johnson went on hiatus from our clinic but returned in 2014 for a hearing test. Test results revealed profound to severe to profound sensorineural hearing loss for the left ear and no aidable response for the right ear. SAT was obtained at 95 dB HL for the left ear, and no response for the right ear. Word recognition score was obtained at 33% at the volume level of 110 dB HL.

Ms. Johnson’s 2014 Audiogram
(Blue X’s= Left Ear, Red O’s=Right Ear)
Ms. Johnson was fitted with a Unitron Max E Super Power (SP) BTE hearing aid. However, she expressed that the hearing aid provided little to no benefit for her left hearing sensitivity. Ms. Johnson expressed she preferred her Phonak Classica PP-C-L-P BTE hearing aid, which was received sometime between the years 2000 and 2014. Ms. Johnson stated that she received more benefits with her Phonak Classica PP-C-L-P BTE hearing aid compared to the Unitron Max E SP BTE.

Unitron Max E SP BTE

Phonak Classica PP C-L-P BTE
2024:
Upon evaluation, Mrs. Johnson underwent comprehensive hearing tests to assess the extent and nature of her hearing loss. Pure-tone audiometry revealed profound bilateral sensorineural hearing loss, with thresholds surpassing 90 dB HL across all frequencies from 250 Hz to 8000 Hz. For the left ear, responses to the pure tone stimuli were obtained at 105 decibels (dB) at 250 Hertz (Hz), 105 dB at 500 Hz, and 115 dB at 750 Hz. There were no measurable responses to the pure tone stimuli beyond 750 Hz for her left ear (no responses from 1000 Hz to 8000 Hz). No measurable responses were obtained across all frequencies for her right ear.
A speech audiometry test revealed that SAT was obtained at 105 dB HL for the left ear, and no measurable responses were obtained for the right ear due to the profound nature of her hearing loss. Word Recognition Score (WRS) could not be obtained due to the profound hearing loss in the right and left ears. This is indicative of significant communication challenges for Ms. Johnson.
Overall, the test results revealed that Ms. Johnson’s left hearing sensitivity decreased significantly in low frequencies compared to her previous test results from 2014. The cause of her decreased hearing sensitivity is unknown.
 Ms. Johnson’s 2024 Audiogram
Ms. Johnson’s 2024 Audiogram
(Blue X’s= Left Ear, Red O’s=Right Ear)
Ms. Johnson received a Phonak Naida P-30 UP BTE hearing aid for her left ear from another clinic facility in the summer of 2023. Her hearing aid was reprogrammed to her 2024 test results and adjusted for better listening comfort. Unfortunately, her hearing aid reached the maximum output limit and caused her left hearing aid to present constant feedback or whistling, even with her new custom-fitted hearing aid earmold.

Phonak Naida P-30 UP BTE
Overall Impressions and Follow-Up and Counseling:
It was noted that since 1992, Ms. Johnson’s hearing sensitivity progressively declined in her left ear, specifically in the low frequencies, with a decreased ability to detect speech and, ultimately, the inability to understand speech at the maximum output level of the audiometer equipment.
Following the hearing tests, Mrs. Johnson received counseling regarding her newly discovered profound sensorineural hearing loss in her left ear, as well as management options. Despite previous success with her left hearing aid, her deteriorating condition calls for the exploration of alternative interventions.
The limitations of digital amplification devices were discussed with Ms. Johnson, and the potential benefits of cochlear implants were highlighted. Mrs. Johnson was initially against obtaining a cochlear implant as she was concerned that, at her age, she may not benefit from such treatment and expressed that she was worried that she would not hear the same as she would with her hearing aid.
Ms. Johnson expressed that her audiologist recommended a cochlear implant evaluation in 2014. She indicated that, at that time, she was not comfortable moving forth with the evaluation and the cochlear implant surgical procedure. It was discussed with Ms. Johnson that even the most powerful hearing aid on the market could no longer provide aidable benefit for her left hearing sensitivity.
It was shared with Ms. Johnson that aural rehabilitation and support from a cochlear implant team may help her once again obtain the ability to hear speech and have sound awareness. She then expressed interest in pursuing further evaluation for cochlear implant candidacy. Ms. Johnson will start the process by obtaining further hearing and medical evaluation with an otolaryngologist and audiologist specializing in cochlear implants.
Clinical Afterthought and Further Hearing and Medical Evaluation Recommendations for Ms. Johnson:
Should Ms. Johnson move forward with obtaining a cochlear implant, there are steps she would need to take to determine cochlear implant candidacy.
Additional assessments should be conducted by an audiologist specializing in cochlear implant candidacy and treatment to determine Mrs. Johnson's suitability for cochlear implants. Speech in noise testing and other recommended speech audiometry evaluations should confirm her significant difficulty in understanding speech, even in optimal listening conditions and using the left hearing aid. These findings, coupled with her audiometric results, should support her candidacy for cochlear implantation.
The audiologist would then recommend that Ms. Johnson obtain a thorough medical evaluation by an otolaryngologist specializing in cochlear implantation. This evaluation would assess her overall health status, cognitive function, and anatomical suitability for surgery. Physical examination and imaging studies should be completed, concluding no contraindications to cochlear implantation, paving the way for further consideration.
Recommendations for Cochlear Implants for Ms. Johnson:
Once collective findings from Ms. Johnson’s assessments were obtained, it should be determined that she would be a suitable candidate for a cochlear implant. The multidisciplinary team, comprising audiologists, otolaryngologists, and cochlear implant surgeons, should collaborate to develop an individualized treatment plan tailored to her needs and preferences.
Conclusion:
Mrs. Johnson's hearing loss journey was quite astonishing. From using hearing aids to being considered for cochlear implants, showcases the significant impact of advanced auditory treatments for severe to profound hearing loss. Despite the hurdles she faced due to her progressive hearing impairment, Mrs. Johnson's story highlights the transformative potential of thorough assessment, counseling, and teamwork among healthcare experts. By embracing these interventions, individuals like Mrs. Johnson can regain access to sound, leading to remarkable improvements in communication and quality of life.
2025/01/05 Update
It is quite important to take a hearing test regularly to understand you actual hearing situation, take now at LINNER Online free hearing test and get result in 5 minutes.
References:
- American Speech-Language-Hearing Association. (2020). Cochlear Implants [Technical Report]. https://www.asha.org/policy/tr2020-00295/
- Centers for Disease Control and Prevention. (2021). Hearing Loss in Older Adults. https://www.cdc.gov/aging/hearingloss/index.html
- Lin, F., Yaffe, K., Xia, J., Xue, Q.-L., Harris, T. B., Purchase-Helzner, E., & Health ABC Study Group. (2013). Hearing loss and cognitive decline in older adults. JAMA Internal Medicine, 173(4), 293–299. https://doi.org/10.1001/jamainternmed.2013.1868
- Zeitler, D. M., Prentiss, S. M., Sydlowski, S. A., & Dunn, C. C. (2024). American cochlear implant alliance task force: recommendations for determining cochlear implant candidacy in adults. The Laryngoscope, 134, S1-S14. https://onlinelibrary.wiley.com/doi/full/10.1002/lary.30879
- Shukla, A., Harper, M., Pedersen, E., Goman, A., Suen, J. J., Price, C., ... & Reed, N. S. (2020). Hearing loss, loneliness, and social isolation: a systematic review. Otolaryngology–Head and Neck Surgery, 162(5), 622-633. https://pubmed.ncbi.nlm.nih.gov/32151193/
- Cuda, D., Manrique, M., Ramos, Á., Marx, M., Bovo, R., Khnifes, R., ... & Mosnier, I. (2024). Improving quality of life in the elderly: hearing loss treatment with cochlear implants. BMC geriatrics, 24(1), 16. https://link.springer.com/article/10.1186/s12877-023-04642-2
- Turton, L., Souza, P., Thibodeau, L., Hickson, L., Gifford, R., Bird, J., ... & Timmer, B. (2020, August). Guidelines for best practice in the audiological management of adults with severe and profound hearing loss. In Seminars in Hearing (Vol. 41, No. 03, pp. 141-246). Thieme Medical Publishers, Inc.. https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0040-1714744
- Davidson, A., Marrone, N., Wong, B., & Musiek, F. (2021). Predicting hearing aid satisfaction in adults: A systematic review of speech-in-noise tests and other behavioral measures. Ear and hearing, 42(6), 1485-1498. 2021.https://journals.lww.com/ear-hearing/fulltext/2021/11000/Predicting_Hearing_Aid_Satisfaction_in_Adults__A.4.aspx?casa_token=FNyS2k3lLMsAAAAA:jKvmwmEQIdiOEu-BUftRfat7SYihAwNMUiZiWkIM03vSn2j4egsw0VhyoiHDSJg-aJv7tGApb2LjB7YIliuuzeu5
- Prentiss, S., Snapp, H., & Zwolan, T. (2020). Audiology practices in the preoperative evaluation and management of adult cochlear implant candidates. JAMA Otolaryngology–Head & Neck Surgery, 146(2), 136-142. https://jamanetwork.com/journals/jamaotolaryngology/article-abstract/2757029
- Zwolan, T. A., & Basura, G. (2021, November). Determining cochlear implant candidacy in adults: limitations, expansions, and opportunities for improvement. In Seminars in Hearing (Vol. 42, No. 04, pp. 331-341). Thieme Medical Publishers, Inc. https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0041-1739283
- Amoodi, H. A., Mick, P. T., Shipp, D. B., Friesen, L. M., Nedzelski, J. M., Chen, J. M., & Lin, V. Y. (2012). Results with cochlear implantation in adults with speech recognition scores exceeding current criteria. Otology & Neurotology, 33(1), 6-12. https://journals.lww.com/otology-neurotology/fulltext/2012/01000/Results_With_Cochlear_Implantation_in_Adults_With.3.aspx?casa_token=-SCZ0HVz6i8AAAAA:P7Hi8okSuyC-JrhUC4-aU9dEAvHbsFEd_bH7UE-OYZAIDLs3Ant97gYvffKLskksT-rqKHJ_1PRJ6MW1e_sZcGCp
- Lansbergen, S., & Dreschler, W. A. (2022). Classification of hearing aids into feature profiles using hierarchical latent class analysis applied to a large dataset of hearing aids. Ear and hearing.
- Buchman, C. A., Herzog, J. A., McJunkin, J. L., Wick, C. C., Durakovic, N., Firszt, J. B., ... & CI532 Study Group. (2020). Assessment of speech understanding after cochlear implantation in adult hearing aid users: a nonrandomized controlled trial. JAMA Otolaryngology–Head & Neck Surgery, 146(10), 916-924.
https://jamanetwork.com/journals/jamaotolaryngology/article-abstract/2769938
***Please Note: To safeguard the individual's privacy, the name has been changed in this article.
***Disclaimer: The content presented here serves general informational purposes and is not intended as professional advice or a replacement for medical consultation. It is essential to seek personalized guidance and assistance from a qualified physician or hearing healthcare provider for any specific questions, concerns, or individual health conditions related to hearing. A professional in the field can offer a comprehensive evaluation and suitable recommendations based on your unique circumstances. Ignoring or postponing seeking medical or professional help may have negative impacts on your health. Always consult with a healthcare professional for precise diagnosis, appropriate treatment, and personalized advice concerning your hearing health.***